The potential role of CT calcium scoring in population screening for cardiovascular disease
About half of patients presenting with myocardial infarction (MI) have no history of coronary heart disease before presenting with their first MI, and about half die from their first event.1 Because such a high proportion of patients experience their first symptoms in the form of an MI or death, there is a strong case for early detection of disease and primary prevention. The current approach to population screening recommended by the National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand,2 and by many national and international bodies around the world, is to treat individuals according to their absolute risk of a cardiovascular event as determined by clinical risk assessment. Most guidelines suggest medical therapy, such as cholesterol lowering, if there is a greater than 2% annual risk of a cardiovascular event. The problem with this approach, however, is that not all high-risk people will have a cardiovascular event, and many low-risk people do. Thus, depending on which cut-off is used to define risk, many heart attacks occur in low-risk people. Therefore, interest has evolved in developing non-invasive tests that are both sensitive and specific for better identifying at-risk individuals.
The test
CT calcium scoring is a simple rapid test in which coronary artery calcium (CAC) is quantified non-invasively through a relatively low-radiation (~1mSv), non-contrast CT. Both electron beam computed tomography (EBCT) and the newer multi-slice computed tomography (MSCT) can be used to quantify CAC. Scans usually take less than 20 seconds to acquire, and the turnaround time for the whole test, including CT evaluation, is approximately 15 minutes. No preparation is required prior to testing, and a quantitative scan is usually achievable even in less than optimal conditions (higher heart rates and arrhythmias), unlike CT coronary angiography.3-5
What is a calcium score?
Coronary artery calcium is defined as being present if at least four contiguous pixels with a CT density of ≥130 Hounsfield units is detected. Most CT scanners have software packages that enable automatic detection of calcium according to this definition (Figure 1). The reproducibility of this technique is good.6
The calcium score is a summation of the CAC measured for all major coronary vessels across multiple images, and is calculated using the Agatston (the more common approach)7 or volume approach. The calcium score is usually reported as a single total patient score with a reference range according to the age and sex of the patient.
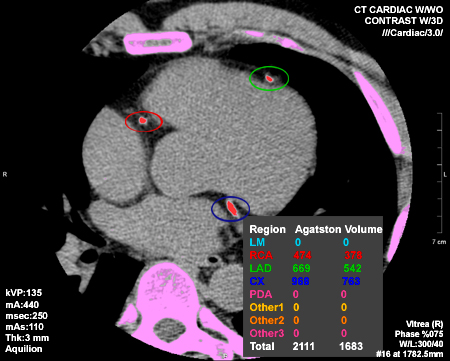 |
Figure 1: Quantification of calcium score – calcium in bones is highlighted in pink, and calcium in coronary arteries in red. |
While certain levels of calcium are clearly pathological at any age (Table 1), the population distribution of coronary calcium is age and sex dependent, and may also vary across ethnic groups.
Table 1: Risk of cardiovascular event with increasing coronary artery calcification
| Score | Description | Relative risk of cardiovascular events |
|---|---|---|
| 0 | No coronary calcification | |
| 1–99 | Mild coronary calcification | 1.9 (95% confidence interval 1.3–2.8) |
| 100–399 | Moderate calcification | 4.3 (3.1–6.1) |
| 400–999 | Severe calcification | 7.2 (5.2–9.9) |
| ≥1000 | Extensive calcification | 10.8 (4.2–27.7) |
Based on information from Greenland et al.4
How common is CAC in the population?
Two recent population-based studies have published CAC centile distribution values: the Multi-Ethnic Study on Atherosclerosis (MESA) in the USA,8 and the Heinz Nixdorf Recall (HNR) study in Germany.9
For men, the mean Agatston CAC scores in the HNR study range from 91 (45-49 yrs) to 577 (70–74 yrs), and for women from 11 (45–59 yrs) to 206 (70–74 yrs). The centile distributions from MESA and HNR are similar; however, in the German population, the curves are shifted to the left and upwards from the age of 65 years. This may be due to the higher prevalence of risk factors in Germany compared with the USA.
The MESA study also demonstrates ethnic variation in CAC. Whites have the highest CAC prevalence, followed by Hispanic, Black and Chinese groups. MESA and HNR both provide internet calculators to enable calculation of a patient’s position relative to others of the same age, gender and (MESA only) race. These can be found at http://www.mesa-nhlbi.org/ and http://www.recall-studie.uni-essen.de/.
What is the relationship of CAC to obstructive coronary disease and cardiovascular events?
The presence of CAC indicates coronary atherosclerosis, but not necessarily significant coronary narrowing. CAC has a high sensitivity and negative predictive power for obstructive coronary disease, but limited specificity. In a study of 1851 patients undergoing angiography and CAC, a negative score was highly associated with no obstruction on angiography (negative predictive power of 98%).10 In the HNR study, of the subset of 327 who had known coronary disease, all of the males and 92.8% of the females had CAC.11
Many heart attacks occur at the site of non-obstructive plaque. A range of studies have examined whether CAC predicts cardiovascular events, and found that the risk associated with any degree of CAC compared with no CAC is increased by a factor of ~4 over the next 3–5 years.12 Higher CAC scores are associated with higher rates of events (Table 1 above), with some studies reporting very high risk of events for those with very high scores. For example, Wayhs and colleagues reported that patients with CAC greater than 1000 experienced a hard cardiac event (MI/death) annual rate of 25%.13
Does CAC add information to conventional risk scores?
A number of studies have shown that CAC does add to the predictive ability of conventional risk scores.14-16 This is particularly useful in groups with intermediate risk on conventional risk scores, as CAC can assist in reclassifying patients in intermediate risk groups to a high risk group and medical therapy, or to lower risk groups in which behavioural management is reasonable.
Does CT calcium scoring have a role in population screening?
CT screening for heart disease in asymptomatic populations currently cannot be justified. There are still a number of issues to resolve. There is no consensus yet on what to do with asymptomatic people who are CAC positive – it is unclear when they should be referred for angiography, or if they all should be treated with cholesterol-lowering. There is no evidence yet that a screening program would be effective in reducing mortality or morbidity. The cost-effectiveness of such programs is also unknown.
There is, however, evidence to support the utility of CAC assessment in those at intermediate risk. A CAC score can effectively reclassify people classified as intermediate on the basis of risk factors, and thus influence clinical decision making. This is the current consensus recommendation by the ACCF/AHA 2007 Clinical Expert Consensus document on coronary artery calcium scoring.4 The panel also states that the current CAC literature does not support the concept that high-risk asymptomatic individuals can be safely excluded from medication therapy for CHD, even if CAC is zero.
Article kindly written by:
Dr Clara K Chow MBBS, FRACP, PhD
Senior Research Fellow; Population Health Research Institute; Hamilton General Hospital, Canada
Editorial Advisory Board Member: Virtual Cardiac Centre.
References:
- Tunstall-Pedoe H, Morrison C, Woodward M, Fitzpatrick B, Watt G. Sex differences in myocardial infarction and coronary deaths in the Scottish MONICA population of Glasgow 1985 to 1991. Presentation, diagnosis, treatment, and 28-day case fatality of 3991 events in men and 1551 events in women. Circulation. 1996; 93(11): 1981-92.
- Tonkin A, Barter P, Best J, Boyden A, Furler J, Hossack K, et al. National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand: Position statement on lipid management – 2005. Heart Lung Circ. 2005; 14(4): 275-91.
- Erbel R, Mohlenkamp S, Kerkhoff G, Budde T, Schmermund A. Non-invasive screening for coronary artery disease: Calcium scoring. Heart. 2007; 93(12): 1620-9.
- Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: A report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2007; 49(3): 378-402.
- Budoff MJ, Gul KM. Expert review on coronary calcium. Vasc Health Risk Manag. 2008; 4(2): 315-24.
- Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, et al. Assessment of coronary artery disease by cardiac computed tomography: A scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006; 114(16): 1761-91.
- Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990; 15(4): 827-32.
- Bild DE, Detrano R, Peterson D, Guerci A, Liu K, Shahar E, et al. Ethnic differences in coronary calcification: The Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2005; 111(10): 1313-20.
- Schmermund A, Mohlenkamp S, Berenbein S, Pump H, Moebus S, Roggenbuck U, et al. Population-based assessment of subclinical coronary atherosclerosis using electron-beam computed tomography. Atherosclerosis. 2006; 185(1): 177-82.
- Budoff MJ, Diamond GA, Raggi P, Arad Y, Guerci AD, Callister TQ, et al. Continuous probabilistic prediction of angiographically significant coronary artery disease using electron beam tomography. Circulation. 2002; 105(15): 1791-6.
- Erbel R, Mohlenkamp S, Lehmann N, Schmermund A, Moebus S, Stang A, et al. Sex related cardiovascular risk stratification based on quantification of atherosclerosis and inflammation. Atherosclerosis. 2008; 197(2): 662-72.
- Waugh N, Black C, Walker S, McIntyre L, Cummins E, Hillis G. The effectiveness and cost-effectiveness of computed tomography screening for coronary artery disease: Systematic review. Health Technol Assess. 2006; 10(39): iii-iv, ix-x, 1-41.
- Wayhs R, Zelinger A, Raggi P. High coronary artery calcium scores pose an extremely elevated risk for hard events. J Am Coll Cardiol. 2002; 39(2): 225-30.
- Taylor AJ, Bindeman J, Feuerstein I, Cao F, Brazaitis M, O’Malley PG. Coronary calcium independently predicts incident premature coronary heart disease over measured cardiovascular risk factors: Mean three-year outcomes in the Prospective Army Coronary Calcium (PACC) project. J Am Coll Cardiol. 2005; 46(5): 807-14.
- Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: The St. Francis Heart Study. J Am Coll Cardiol. 2005; 46(1): 158-65.
- Park R, Detrano R, Xiang M, Fu P, Ibrahim Y, LaBree L, et al. Combined use of computed tomography coronary calcium scores and C-reactive protein levels in predicting cardiovascular events in nondiabetic individuals. Circulation. 2002; 106(16): 2073-7.
Dates
Tags
Created by:

 Login
Login














