Somatosensory Evoked Potential (SSEP)
- What is a somatosensory evoked potential (SSEP)?
- When is the SSEP used?
- What does the SSEP detect?
- How to prepare for a SSEP test
- What happens during a SSEP test?
- Side effects
- Factors influencing the SSEP
- What the results of the SSEP may show
- Clinical usefulness of the SSEP
- Summary of SSEP
What is a somatosensory evoked potential (SSEP)?
 A somatosensory evoked potential (SSEP) is an evoked potential caused by a physical stimulus (usually a small electric pulse). Electrodes positioned over particular areas of the body record responses of the SSEP, these are then observed as a reading on an electroencephalogram (EEG). A SSEP can most commonly involve stimulation of the median nerve at the wrist, or the posterior tibial nerve at the ankle. This investigation therefore tests the pathway of the sensory nerves to the sensory areas of the brain, even though the stimuli are non-physiological.
A somatosensory evoked potential (SSEP) is an evoked potential caused by a physical stimulus (usually a small electric pulse). Electrodes positioned over particular areas of the body record responses of the SSEP, these are then observed as a reading on an electroencephalogram (EEG). A SSEP can most commonly involve stimulation of the median nerve at the wrist, or the posterior tibial nerve at the ankle. This investigation therefore tests the pathway of the sensory nerves to the sensory areas of the brain, even though the stimuli are non-physiological.
When is the SSEP used?
A doctor may recommend you go for a SSEP test if you have been experiencing feelings of numbness or weakness in your arms or legs that may be due to problems affecting the somatosensory nerve pathway. These feelings are often very subtle and not easily detected in a routine clinical examination.
What does the SSEP detect?
From the SSEP, a neurologist is able to determine the time it takes for nerve fibres to relay a stimulus from the point of stimulation (wrist or ankle) to a detection site on the scalp, neck or back. By analysing the SSEP pattern, the neurologist can get an idea of how well these sensory nerves are working. Multiple sclerosis (MS) for example, can damage the myelin sheath insulating nerve fibres of the brain and spinal cord in a process called demyelination. The damage means it takes a longer time for signals to be relayed along nerve pathways, or they may be blocked, resulting in changes in the SSEP.
How to prepare for a SSEP test
If you have a pacemaker, you should let the person conducting the test know before you begin.
- Eating a normal meal before the procedure should be fine.
- Please bring a list of your medication with you. Sedatives and drugs that can make you drowsy should be avoided.
- Arrive at the test on time and try to relax.
- No further preparation should be necessary.
What happens during a SSEP test?
The SSEP procedure itself is safe and non-invasive. You may be asked to remove your shoes and outer upper garments to allow the placement of electrodes.
- Some detection electrodes will be glued to particular spots on your scalp, neck and back.
- A small generator is used to create tiny electrical impulses that are used to stimulate nerves in the wrist or the ankle. While the impulses are usually not painful, they may cause your thumb or toe to twitch a little, which is normal.
- In order for the test to be accurate, it is very important that you listen carefully to the person conducting the test, follow their instructions, and try to relax where possible.
- Responses to the electrical stimulation are recorded through the electrodes using special equipment.
- After the procedure the electrodes will be removed and you will be able to put your clothes and shoes back on.
- Unless instructed otherwise, you should be able to go straight home after the procedure.
- Your doctor may discuss the results of the test with you after they have been analysed; otherwise the referring doctor will.
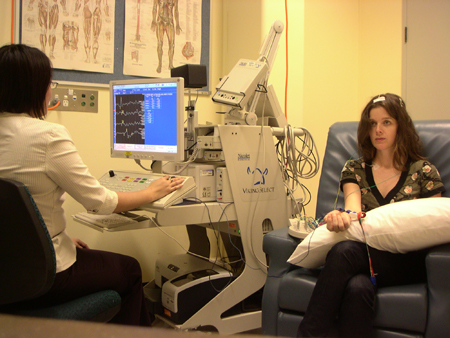 |
| (Image courtesy of Dr K Ng) |
Side effects
The SSEP testing procedure is usually painless; the electrical impulses used as the stimulus are very small. Side effects from the procedure are very rare, though there is a chance you may have some minor skin irritation from the electrodes. Given that you are well enough, you should be able to drive yourself home after the procedure.
Factors influencing SSEPs
Your age, gender, height, limb length, and body temperature are factors that can influence SSEP readings.
Some drugs may affect the SSEP.
What the results of the SSEP may show
 SSEPs can helpful in the diagnosis of:
SSEPs can helpful in the diagnosis of:
- Trauma – any physical injuries affecting nerves and nerve pathways of the somatosensory system.
- Tumours – these can affect the nerves involved in relaying signals of the somatosensory system.
- Multiple sclerosis (MS) – Damage to nerve fibres in the body is a common feature of MS. SSEP analysis can help in the confirming and localising areas affected by the disease.
- Myoclonus – this refers to the twitching of a muscle or muscle group. Myoclonus can develop in response to a physical injury or stroke but is often a symptom associated with another neurological condition.
- Dystonia – this is a condition that is characterised by an involuntary sustained muscle contraction.
- Metabolic problems such as vitamin B12 deficiency can produce changes in a SSEP.
- A variety of neurological disorders can affect the SSEP.
- Hereditary neuropathies such as Charcot-Marie tooth disease and Friedreich ataxia.
Clinical usefulness of the SSEP
- SSEP analysis can be an accurate technique in measuring sensory conduction
- An SSEP test can inform us about the presence and extent of a particular disease or injury affecting the somatosensory nerve system.
- It can be used to monitor someone’s neurological condition and thus track disease progression.
- It is often less costly than other techniques such as an MRI
- SSEP analysis is also used to monitor a patient’s status during surgery near the spinal cord, or in the intensive care unit (ICU) for brain injury.
- It is often less costly than other techniques such as an MRI
Summary of SSEP
Testing the somatosensory evoked potential (SSEP) involves monitoring responses to physical stimulation at the wrist or ankle using electrodes placed on the scalp, neck or back. It is a useful test that can detect problems associated with nerves of the somatosensory system. They can help in localising areas affected by diseases such as multiple sclerosis and also monitor changes in a patient’s neurological process.
Article kindly reviewed by:
Associate Professor Karl Ng MB BS (Hons I) FRCP FRACP PhD CCT Clinical Neurophysiology (UK) Consultant Neurologist – Sydney North Neurology and Neurophysiology (download referral form and map); Conjoint Associate Professor – Sydney Medical School, University of Sydney; and Editorial Advisory Board Member of the Virtual Neuro Centre.
References
- Walsh P, Kane N, Butler S. The clinical role of evoked potentials. J Neurol Neurosurg Psychiatry. 2005;76 Suppl 2:ii16-22. [Full text]
- Nicholas JF, Samra SK. Sensory evoked potentials. Semin Anesth. 1997;16(1):14-27. [Abstract]
- Nuwer MR. Fundamentals of evoked potentials and common clinical applications today. Electroencephalogr Clin Neurophysiol. 1998;106(2):142-8. [Abstract]
- Somatosensory evoked potentials (SSEP) [online]. Los Angeles: Cedars-Sinai Health System; 2008 [cited February 2008]. Available from: [URL link]
- Ng K, Jones S. The “enhanced N35” somatosensory evoked potential: Its associations and potential utility in the clinical evaluation of dystonia and myoclonus. J Neurol. 2007;254(1):46-52. [Abstract]
- Deuschl G, Eisen A (eds). Recommendations for the Practice of Clinical Neurophysiology: Guidelines of the International Federation of Clinical Neurophysiology. Electroencephalogr Clin Neurophysiol Suppl. 1999;52:1-304. [Abstract]
Dates
Tags
Created by:

 Login
Login














