Skin Biopsy
Introduction
A skin biopsy is often a simple procedure that can be performed by your General Practitioner. Skin biopsies can be important in determining the type of lesion/skin condition (diagnosis) and can even be the only treatment that is required for some lesions.
Skin biopsies can be performed for a number of different skin conditions. They are commonly performed for skin lesions that are suspicious of cancers (e.g. basal cell carcinoma (BCC), squamous cell carcinoma (SCC) and/or melanoma) but also for a range of other skin conditions.
Skin biopsies can be broadly classified into two main groups:
- incisional – where only a part of the lesion is sampled, this includes: shave biopsies, partial punch biopsies or surgical incisional biopsies; and
- excisional – remove the entire lesion such as surgical excisional biopsy and/or punch biopsy (if the lesion is relatively small and can be completely excised by this method).
The type of biopsy used depends on where it is located, how big it is and what shape it is.
Shave biopsy

Shave biopsies are ideal for lesions that are thin and are spread over a large area. The technique involves firstly cleaning and anaesthetising the skin. Either a scalpel, a double edged blade or a pair of scissors is then used to shallowly remove a thin disc.
Shave biopsies have the advantage that they avoid the use of sutures (stiches) and often heal so well that once healed it may be difficult to determine where the biopsy was taken from. Shave biopsies aren’t performed if there is any suspicion that it may be a melanoma.
Punch biopsy
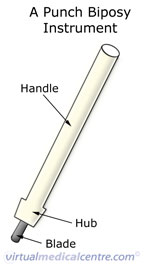
A punch biopsy makes use of a punch biopsy instrument that consists of circular blade attached to a pen-like handle. Different sizes are available (they vary in the diameter of the circular blade) and the blade can be inserted to varying depths within the tissue. This is performed with the skin cleaned and anaesthetised. In some situations a suture (stitch) may be required to help it heal.
A punch biopsy may be used for incisional or excisional biopsies depending on the size of the lesion and the size biopsied. For example, if a lesion is relatively small the entire lesion may be able to be removed with this method (excisional biopsy). If the lesion is relatively large, the entire lesion may not be able to be removed with this method and only a portion can be biopsied (incisional biopsy).
Surgical biopsy
 If you or your doctor are worried that a skin lesion may be a skin cancer (a melanoma or a non-melanoma skin cancer) then an excisional surgical biopsy is recommended. Where a skin cancer is suspected, the lesion as well as an area around the lesion (surgical margin) will be removed. The amount of tissue around the lesion that needs to be removed can vary depending on the type of lesion that is suspected.
If you or your doctor are worried that a skin lesion may be a skin cancer (a melanoma or a non-melanoma skin cancer) then an excisional surgical biopsy is recommended. Where a skin cancer is suspected, the lesion as well as an area around the lesion (surgical margin) will be removed. The amount of tissue around the lesion that needs to be removed can vary depending on the type of lesion that is suspected.
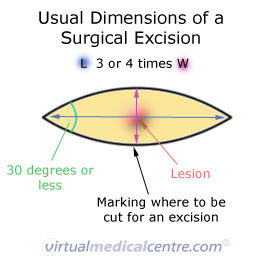
There are many different ways to perform a surgical biopsy. One method involves cleaning the skin and then marking out the lesion boundary and the excision lines with a marker. The skin can then be anaesthetised and the lesion excised with a scalpel. The wound will then require suturing (stitches). The length of time that the sutures stay in vary depending on the location that they are placed e.g. sutures on the face don’t stay in as long as sutures on the back or legs.
After the biopsy
Once the skin biopsy has been performed, the wound is usually cleaned and a dressing applied. In some cases an antibiotic is applied to the wound, however, this is not required for most skin biopsies. It is important to ask your doctor performing the skin biopsy:
- How often should I change the dressing?
- If I am unable to change the dressing or provide wound care myself, is there a service available to assist me?
- Can I get the wound wet? i.e. can I shower/bath/swim
- Can I exercise while the wound is healing?
- Are there any creams, lotions or ointments that are recommended?
- How can I minimise scarring?
These are all very important questions related to the care of your wound. The answers to them will vary depending on the site, size and type of biopsy performed as well as your doctor’s professional preference and the services available in your community.
Skin biopsies are generally performed under local anaesthetic. This involves injecting anaesthetic into the site prior to biopsy so that the area becomes numb. When local anaesthetic is used you remain awake during the procedure. Depending on the site and the extent of the biopsy you may or may not be able to drive home following the procedure. It is best to discuss this with your doctor prior to the procedure. It may be that if a large area is being biopsied and/or a site that is essential for your driving ability, it may be advisable not to drive.
Larger more complex biopsies performed in a surgical theatre may require the use of a general anaesthetic. This may be performed as an inpatient (i.e. you get admitted to the hospital overnight or longer) or as a day case in which you can go home the same day. If a general anaesthetic is used, even if you can go home the same day, you will not be able to drive and will need someone to stay with you for at least 24 hours afterwards. You should discuss this with your doctor prior to surgery so appropriate plans can be made.
After a skin biopsy is taken, it usually takes at least two weeks for the results to become available with the exception of some urgent cases. Different doctors have different professional preferences, some like to book you in for your next appointment before you leave while others will wait until your results are available and then phone to arrange an appointment. When you return for your follow-up appointment, your doctor can then discuss the results with you and any follow-up that may be needed.
Kindly written and reviewed by Dr Allison Johns Bsc (Hons) MBBS, Doctor at Child and Adolescent Health Services, Women and Newborn Health Services and Editorial Advisory Board Member of Virtual Medical Centre.
References
- Pickett H. Shave and Punch Biopsy for Skin Lesions. Am Fam Physician 2011; 84(9): 995-1002. Available from: [PDF File]
- Clarke P. Nonmelanoma skin cancers: treatment options. Australian Family Physician 2012; 41(7): 476-480. Available from: [URL Link]
- Australian Cancer Network. ‘Clinical Practice Guidelines for the management of melanoma in Australia and New Zealand’ (online), Cancer Council of Australia, 2008 [Accessed 30th October 2014]. Available from: [PDF File]
- Australian Cancer Network. Management of Non-Melanoma Skin Cancer Working Party. ‘Clinical Practice Guidelines Non-melanoma skin cancer: Guidelines for treatment and management in Australia’, Cancer Council of Australia, 2003. Available from: [PDF File]
- Australian Cancer Network. ‘Clinical Practice Guide: basal cell carcinoma, squamous cell carcinoma (and related lesions) – a guide to clinical management in Australia’. November 2008 [Accessed 2nd December 2014]. Available from: [PDF File]
Dates
Tags
Created by:

 Login
Login














