Core Biopsy
- Introduction to core biopsy
- How is a core biopsy done?
- Results of a core biopsy
- How effective are core biopsies?
- Benefits and risks of a core biopsy
- Core biopsy or fine needle aspiration biopsy?
Introduction to core biopsy
 A core biopsy is a procedure where a needle is passed through the skin to take a sample of tissue from a mass or lump. The tissue is then examined under a microscope for any abnormalities.
A core biopsy is a procedure where a needle is passed through the skin to take a sample of tissue from a mass or lump. The tissue is then examined under a microscope for any abnormalities.
Core biopsy may be performed when a suspicious lump is found, for example a breast lump or enlarged lymph node, or if an abnormality is detected on an imaging test such as x-ray, ultrasound or mammography.
Core biopsy is a more invasive procedure than fine needle aspiration biopsy, as it involves a local anaesthetic. However, it is quicker and less invasive than a surgical biopsy. In some cases, the result of a core biopsy will prevent the need for surgery to take place.
How is a core biopsy done?
A core biopsy is a simple procedure, performed to collect a sample of cells from a mass so they can be examined under a microscope.
No special preparation is required, though most centres ask that you don’t use any powders (such as talcum powder), lotions, creams, perfumes or deodorants near the area to be sampled.
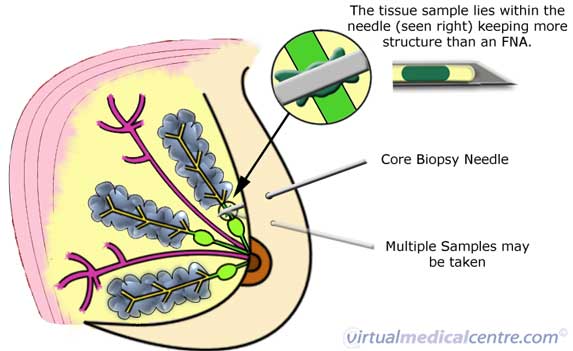
Core biopsy is performed with the use of local anaesthetic to numb the area where the needle is inserted. A small incision (cut) is made in the skin over the lump, and a needle is inserted through the incision. When the tip of the needle is in the area to be examined, the specially-designed hollow needle is used to collect a sample of the cells that are present. This is shown in the diagram below. The needle is then withdrawn, and the sample extracted. This may be repeated up to 5 times, until an adequate sample has been collected.
Information on re-publishing of our images
In some cases, the lump or mass from which the cells are to be taken is not easily felt through the skin. If this is the case, the radiologist, surgeon or pathologist collecting the sample may use ultrasound, where the needle can be seen on the ultrasound monitor and guided to the area, or stereotactic mammography (for the breast) which uses two mammograms at different angles and a computer to locate the correct area. This may make the procedure take a little longer. Overall, core biopsy usually takes between 30 minutes to 1 hour to complete.
Because local anaesthetic is used, core biopsy should not be painful, though it may be uncomfortable.
Once the test is completed, a small dressing or some tape will be placed over the biopsy site. This can be removed the next day. Core biopsy may leave a very small, fine scar, which usually fades with time.
There are generally no complications with this procedure, though you may experience some tenderness or bruising over the needle insertion site. If you experience any bleeding, swelling, fever or pain that is not relieved with paracetamol, contact your doctor immediately. It is not recommended that you use aspirin to relive pain as it may worsen any bruising.
Results of a core biopsy
The samples taken are examined by a pathologist under a microscope. A detailed report will then be provided about the type of cells that were seen, including any suggestion that the cells might be cancer. It is important to remember that having a lump or mass does not necessarily mean that it is cancerous; many core biopsies reveal that suspicious lumps or masses are benign (non-cancerous).
Aspirate samples may be described as one of the following types:
- Inadequate/insufficient: The sample taken was not adequate to exclude or confirm a diagnosis of cancer.
- Benign: There are no cancerous cells present. The lump or growth is under control and has no spread to other areas of the body.
- Atypical/indeterminate, or suspicious of malignancy: The results are unclear. Some cells appear abnormal but are not definitely cancerous. A surgical biopsy may be required to adequately sample the cells.
- Malignant: The cells are cancerous, uncontrolled and have the potential or have spread to other areas of the body.
How effective are core biopsies?
 Core biopsy is a quick and effective tool in evaluating and diagnosing suspect lumps or masses. The results of a core biopsy usually take only days to return. This may allow a quick diagnosis, meaning that cancer is detected early, giving more options for treatment. Core biopsy is also very good at determining whether a lump is benign (non-cancerous), potentially avoiding the need for surgery.
Core biopsy is a quick and effective tool in evaluating and diagnosing suspect lumps or masses. The results of a core biopsy usually take only days to return. This may allow a quick diagnosis, meaning that cancer is detected early, giving more options for treatment. Core biopsy is also very good at determining whether a lump is benign (non-cancerous), potentially avoiding the need for surgery.
Core biopsies do require some expertise to perform and interpret. To ensure that an accurate result is achieved, it is important that the radiologist, surgeon, pathologist or oncologist who performs your procedure has experience in core biopsy.
Benefits and risks of a core biopsy
A core biopsy is a relatively quick and effective test for determining the status of suspect tissue. Compared to a surgical biopsy, core biopsy involves little possibility of scarring, infection or pain, and has a significantly shorter recovery time.
Core biopsies are particularly useful for investigating abnormalities detected on imaging tests, such as x-ray. It is the investigation of choice when breast microcalcification is seen on mammography. Also, because the needle used is large enough to take a coherent ‘slice’ of tissue, it allows the cells to be examined under the microscope as they were arranged in the body. This can help to distinguish between some types of pre-cancerous disease (such as ductal carcinoma in situ) and invasive ductal carcinoma.
The risks of core biopsy include the possibility that any cancer cells present could be trailed into unaffected tissue as the needle is removed, but this is rare when the test is performed by skilled practitioners. If it is thought that a lump to be investigated is likely to be cancerous, the biopsy approach can be arranged so that any cells which may have been spread along the needle tract are easily removed during later surgery.
Core biopsy or fine needle aspiration biopsy?
Fine needle aspiration biopsy is another method of ’tissue diagnosis’ – that is, a way of sampling the cells in a suspicious lump or mass. During the investigation of a breast lump, one or other of the techniques is usually used. The choice of technique is based on a number of factors, including the type or location of the mass to be sampled, the equipment available, and the experience of the operator.
Fine needle aspiration biopsy is slightly quicker and less invasive than core biopsy. Fine needle aspiration biopsy does not require local anaesthetic as the needle is much finer. As with core biopsy, ultrasound or mammographic guidance may be needed to locate the lump or area to be sampled if it cannot be easily felt.
Fine needle aspiration biopsy is more difficult to interpret than core biopsy. This is because the same of cells collected by the fine needle appears under the microscope as a disorganised jumble. It is not possible to distinguish between in situ and invasive cancer on the basis of fine needle aspiration biopsy alone.
More information
 | For information on breast cancer, types of breast cancer and its investigations and treatments, as well as some useful videos, see Breast Cancer. |
References
- Britton PD. Fine needle aspiration or core biopsy. Breast. 1999; 8: 1-4.
- National Breast Cancer Centre. Breast fine needle aspiration cytology and core biopsy: a guide for practice [online]. 2004 [cited 1 January 2007]. Available from URL: http://www.nbcc.org.au/ bestpractice/ resources/ FNA_fineneedleaspir.pdf
- National Breast Cancer Centre. Clinical practice guidelines for the management of early breast cancer (second edition) [online]. Camperdown, NSW: National Breast Cancer Centre. 2001 [cited 1 January 2007]. Available from URL: http://www.nhmrc.gov.au/ publications/ synopses/ cp74syn.htm
- National Breast Cancer Centre. The investigation of a new breast symptom: A guide for general practitioners [online]. 2006 [cited 16 February 2007]. Available from URL: http://www.nbcc.org.au/ bestpractice/ resources/ IBS172_theinvestigationofan.pdf
Dates
Tags
Created by:

 Login
Login














