Cardiac PET Scan (Positron Emission Tomography)
- What is a cardiac PET scan?
- How does a cardiac PET scan work?
- During a cardiac PET scan
- Benefits of a PET scan
- Risks of a cardiac PET scan
- Limitations of a cardiac PET scan
- Results of a PET scan
What is a cardiac PET scan?
A Cardiac PET Scan is an investigation that uses the position of radioactive substances within the body to give an idea about its function. Those parts of the body that are the most active need energy, and the energy that it uses is sugar (also called glucose). A PET scan uses a specially created substance that the body thinks is sugar, and takes it up into the cells. This substance is called a ‘tracer’, and it is almost exactly like sugar, but has a small radioactive part attached to it.
A Cardiac PET Scan uses this same technique, but uses different tracers and some different techniques to get a good idea about the function and blood flow to the heart. Often it is combined with a CT scan so that the doctor can see both the structure and function of the heart.
How Does a Cardiac PET Scan Work?
 PET scans work to identify the cellular changes that occur in the body during disease.
PET scans work to identify the cellular changes that occur in the body during disease.
During a PET scan, the patient is given a substance called a tracer, typically a chemical found in the body (oxygen, glucose, nitrogen, fluorine) which has been tagged with a radioactive atom that breaks down quickly to release positrons. The most common tracer for normal, non cardiac, PET scans has a complicated name but is mostly known as FDG (which stands for 2-[18F]fluoro-2-deoxy-D-glucose). FDG is very similar to glucose (sugar).
Once in the body FDG travels to the area of the body that is using a lot of sugar and breaks it down. In breaking down, it releases a positron. This combines with an electron from the patient sending out radioactive waves.
These waves can be detected by the PET Scanner which converts the waves into electrical signals that can be analysed by a computer. The computer can then create images of the targeted tissue’s function, in a colour code. Different colours or degrees of brightness on a PET image represent different levels of tissue or organ function. In the image to the right, areas that use more sugar, and so collect more of the radioactive substance, are shaded darker.
For example, because healthy tissue uses glucose for energy, it accumulates some of the tagged glucose, which will show up on the PET images. However, cancerous tissue, which uses more glucose than normal tissue because it is growing much faster, will accumulate more of the substance and appear brighter than normal tissue on the PET images.
Therefore PET scans are commonly used to detect cancer, as the scan will detect biochemical changes in the body associated with cancer as well as the extent of spread and the possible effective treatment. Functions of the brain may also be examined in association with patients with memory loss, suspected or known brain tumours or seizure disorders.
For a Cardiac PET Scan, a different tracer is used than in a normal PET scan because uptake of sugar is not a very helpful thing to measure for the heart. For cardiac PET scans, the most common tracers are a type of ammonia with a bit of radioactive material attached to it, a substance called Rubidium and a radioactive type of Fluorine.
During a Cardiac PET Scan
PET scans are generally done in an outpatient setting and preparation is usually set by your doctor. The scan does require the patient to lie still for a period of time for up to two hours, so if you feel you may have a problem with this, please talk to your doctor.
Women who suspect they may be pregnant or are pregnant need to notify their doctor as this is a radioactive procedure and could have effects on an unborn foetus.
The PET scanner is a donut-ring shaped apparatus with an attached table that moves into the scanning ring. Initial scans may be done before you are taken into a special injection room where the tracer is administered, usually intravenously.
It will then take 30-90 minutes for the substance to travel through your body and accumulate. During this time you may be asked to rest quietly to allow the substance to travel through the body. You will then be asked to lie still on the scanner table and it will move in through the scanner ring.
During the scan, which can take from thirty minutes to two hours, you must lie very still to allow for clarity of the images. After the scan there are no restrictions to daily activity, but it is recommended you drink plenty of water to flush your system of the tracer.
Benefits of a PET Scan
PET scans are beneficial as they demonstrate the biochemical changes in the body, whereas a CT or MRI scans identify anatomical changes.
A PET Scan therefore helps to identify problems at the level of their activity and function, which might change long before any changes in body structure (such as a tumour) become apparent.
This allows for earlier diagnosis and more effective treatment of diseases such as cancer, and also more detailed imaging of other conditions. There is little risk involved with the intravenous administration of the radioactive “tracer” as the tracer has a short decay time of only a few hours and is quickly removed from the body.
A cardiac PET scan is useful because it can give very precise images, is not greatly affected by the fast changing blood flow in the heart and can give information about how much of the tracer ends up in different parts of the heart. This is important because it can give doctors information about damage to the heart, and show areas that may have problems with low amounts of blood flow.
Risks of a Cardiac PET Scan
The risks associated with a PET scan are very small, and are due to reactions to the radioactive “tracer” injected. The level of tracer given to a patient is very tiny, and the chances of a reaction occurring are incredibly low.
Limitations of a Cardiac PET Scan
- PET scans can sometimes show areas of high activity which may be mistaken for cancers. Inflammatory conditions like rheumatoid arthritis or tuberculosis absorb a large proportion of the tracer, and so can cause confusing results.
- A PET scan is less accurate in certain situations:
- Slow-growing, less active tumours may not absorb much tracer.
- Small tumours (less than 7mm) may not be detectable.
- High levels of blood sugar can cause the cells to absorb this normal sugar rather than the radioactive, injected kind. Patients are usually fasted for 4 hours before a PET scan, and blood sugar levels measured to lower the chances of this happening.
- The radioactive substance has a very short decay and therefore appointments must run on schedule.
- PET scans are a very expensive form of imaging, and are not readily available. They often accompany other scans such as CT and MRI in order to be diagnostically effective.
Results of a PET Scan
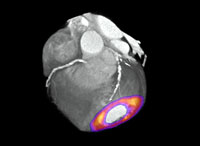 After a PET scan, the doctor will receive an image of the patient displaying the different amounts of activity present in different parts of the body. An image of a combined CT and PET scan is seen to the right. Different colours represent different levels of tracer and so can show different levels of blood flow.
After a PET scan, the doctor will receive an image of the patient displaying the different amounts of activity present in different parts of the body. An image of a combined CT and PET scan is seen to the right. Different colours represent different levels of tracer and so can show different levels of blood flow.
For a normal PET scan, if there is cancer present in the body, this area will appear to be more active and so PET scans are often used to determine if a cancer has spread to other parts of the body, or to see how advanced a cancer is. A PET scan is not as accurate for very small cancers however, so very early scans may not show anything.
Cardiac PET scans could show a doctor that blood flow to the heart is completely normal but could also show that things are going wrong. The doctor would be looking for any parts of the heart that did not get an adequate amount of the tracer as this would show that it is also not getting enough blood.
References
- Di Carli MF, Dorbala S. Integrated PET/CT for cardiac imaging. The Quarterly Journal of Nuclear Medicine and Molecular Imaging, 2006; 50, 1: 44.
- Positron Emission Tomography: Assessment Report. Medicare Services Advisory Committee, 2000. Commonwealth of Australia.
- Khorsand A, Graf S, Eidherr H, Wadsak W, et al. Gated Cardiac 13N-NH3 PET for Assessment of Left Ventricular Volume. The Journal of Nuclear Medicine, 2005; 46 (12): 2009.
Soben P, Udelson KE. ‘Thoracic Assessment of myocardial viability by nuclear imaging in coronary heart disease’ [online],
- UpToDate, 2006. Available at URL: http://www.uptodate.com (last accessed 13/07/06)
- Stark P. ‘Thoracic positron emission tomography’ [online], UpToDate, 2006. Available at URL: http://www.uptodate.com (last accessed 13/07/06)
Dates
Tags
Created by:

 Login
Login