Cardiac MRI (Magnetic Resonance Imaging)
- What is cardiac MRI?
- What is MRI?
- How does the MRI scanner work?
- What will the MRI examination involve?
- Contraindications and risks of cardiac MRI
- The benefits of cardiac MRI
What is cardiac MRI?
| MRI stands for magnetic resonance imaging, a diagnostic technique that uses harmless radio waves rather than x-rays to create images.Cardiac magnetic resonance imaging (CMR) is currently the most accurate and reproducible technique for imaging the heart. It has outstanding image resolution and intrinsic tissue contrast. CMR is safe, non-invasive, and does not expose patients to ionising radiation. Sometimes a contrast dye is injected into the veins to highlight certain features that would not otherwise be visible. |
What is MRI?
| MRI is a safe and painless means of looking inside the body without using radiation. Detailed pictures of the body can be produced by using a large magnet, radio waves, and a computer, often providing information that could not be obtained from other investigations (e.g. x-rays or ultrasound). |  |
How does the MRI scanner work?
The body is made up of small particles called atoms. Hydrogen atoms, a major component of water, make up 95% of your body. Normally, the hydrogen atoms within your body spin around at random. However, when a patient lies within the bore (the central tunnel) of a large, strong magnet, the same hydrogen atoms naturally line up and all spin in the same direction. When a radio wave is passed through the body, it causes the hydrogen atoms to give off signals. The scanner detects these signals and, with the aid of a computer, they are reconstructed into images of the body.
Until recently, clear pictures of the beating heart could not be obtained due to the heart’s constant movement. To overcome this, cardiac MRI uses ECG gating. This allows the scanner to coordinate the pictures with the movement of the heart.
What will the MRI examination involve?
Patients are asked to change into a medical gown. As the magnetic field will damage credit cards, mobile phones and any electronic equipment, these must be left outside the scan room, along with all jewellery and clothing with metal (e.g. zips or jean rivets). The machine will make loud knocking noises while scanning, so patients are often provided with head phones which act as ear protectors and allow them to listen to music during the procedure. The patient lies down on a sliding ‘table’ and ECG electrodes are attached, before they are moved into the scanner.
The scan can last from 30 minutes to an hour. Patients may be asked to hold their breath for 10-20 seconds during some imaging sequences. The patient should remain motionless in order to produce a clear picture. Throughout the examination, radiographers are able to communicate with the patient via intercom to ensure that the patient is informed and comfortable.
Contraindications and risks of cardiac MRI
There are several contraindications to MRI. In particular, patients who have implanted medical devices (e.g. pacemakers or defibrillators, cochlear implants, cerebral aneurysm clips), or who may have iron fragments in their eyes, are not suitable for MRI investigation. Orthopaedic pins, mediastinal clips, coronary stents, and the majority of artificial heart valves are safe to scan.
There are no known risks from undergoing MRI during pregnancy. However, as with any medical investigation, a patient who suspects that she is pregnant should seek advice on the risks versus benefits of undergoing the investigation.
Around 4% of patients will suffer from claustrophobia to a degree that will not allow them to tolerate a MRI scan. This can be reduced to < 2% by sedating with oral or IV benzodiazepines.
There is also the risk of patients being injured if they forget to remove pieces of metal from their person or clothing. If sedation is required, there are associated risks of overmedication. If a contrast dye is used, there is a small risk of an allergic reaction, although this risk is very low.
The benefits of cardiac MRI
The MRI scan is a painless and safe scan that produces clear images of the body, from any angle. The pictures are clearer than those obtained by most other techniques, including both echo and SPECT scanning. It uses no radiation and therefore eliminates the substantial x-ray doses of cardiac CT.
Cardiac MRI is useful in a wide variety of cardiac conditions. It can demonstrate the structure and function of cardiac chambers, and help quantify the flow of blood through the cardiac valves. It is particularly valuable for assessing abnormal heart muscle (cardiomyopathy) and the damage done by previous heart attacks.
Limitations of cardiac MRI
While MRI provides a very high standard image, it is time consuming and more expensive than some other investigations. Very obese patients may not be able to fit comfortably within the MRI machine, and patients with severe heart failure may struggle to lie flat for the duration of the test. Some patients will suffer from claustrophobia to a degree that will not allow them to tolerate a MRI scan. In patients with very fast heart rates, or frequent irregular beats, ECG gating can prove unreliable.
Indications for cardiac MRI
Although not yet widely available in many regions of Australia, cardiac MRI is an established technique in many countries for the diagnosis and management of diseases of the cardiovascular system.
The uses of a cardiac MRI include:
Aortic disease
Cardiac MRI accurately displays the size and shape the aorta. The lack of radiation makes cardiac MRI ideal for repeated examinations, such as the evaluation of patients with Marfan’s syndrome and aortic dilatation, or serial review of coarctation as is seen in the image on the right. Cardiac MRI can also be used for the quantification and characterisation of cholesterol plaques in the major arteries.
Ischaemic heart disease
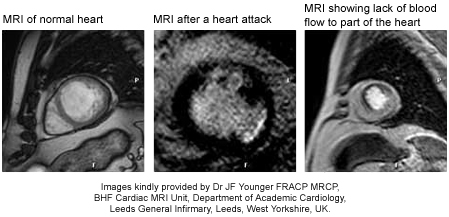
There are multiple approaches to detecting coronary artery disease by cardiac MRI. Blood flow can be assessed at rest and under stress to demonstrate significant coronary blockages. Due to the higher resolution, cardiac MRI may be able to detect smaller areas of ischaemia than would be visible by nuclear scanning. This high resolution also allows detection of wall motion abnormalities, which may affect the heart’s function.
Cardiac MRI can be used for determining the presence, size and location of a heart attack by the technique of delayed enhancement. Delayed enhancement accurately defines myocardial scar, and provides a reliable method to assess the likelihood of recovery of heart function after bypass surgery. It can also be helpful in deciding the cause of heart failure. Coronary arteries can be visualized by cardiac MRI, and coronary stenoses can be demonstrated. It is also possible to assess the flow within the coronary arteries.
Cardiomyopathy
While echocardiography is still the mainstay of diagnosis in cardiomyopathies, cardiac MRI can be used to demonstrate the abnormalities in heart muscle and function, particularly those associated with cardiomyopathies. In particular, cardiac MRI is useful in the diagnosis and follow-up of arrhythmogenic right ventricular dysplasia.
Cardiac masses
Echocardiography remains the initial diagnostic tool for the assessment of cardiac masses, particularly thrombus or tumour. Unlike an echocardiogram, cardiac MRI can easily differentiate between these two diagnoses. It is also useful in the classification of cardiac tumours.
Valvular heart diseases
Cardiac MRI can now be used to clearly assess valvular heart diseases (e.g. narrowed or leaky heart valves), and any damage they have caused to the heart.
Pericardial disease
The pericardium is a fibrous sack that surrounds the heart. An MRI can show any changes to the structure of this sack, and help decide the difference between diseases of the pericardium and of the heart muscle.
Congenital heart diseases
Cardiac MRI is used to give detailed information about the structure and function of the heart in cases where there have been problems with the heart’s development. A cardiac MRI can also be used to give an idea of how and where blood is flowing, which can often be very complicated.
Other
CMR is useful in a wide variety of other cardiac diseases, including left ventricular non-compaction, infiltrative cardiomyopathy and myocarditis. In siderotic cardiomyopathy, caused by iron deposition, myocardial biopsy can be avoided by the use of cardiac MRI.
(Kindly reviewed by Dr JF Younger FRACP MRCP, BHF Cardiac MRI Unit, Department of Academic Cardiology, Leeds General Infirmary, Leeds, West Yorkshire, UK.)
References
- Anderson LJ, Holden S, Davis B, et al. Cardiovascular T2* magnetic resonance for the early diagnosis of myocardial iron overload. Eur Heart J. 2001; 22: 2171-9.
- Bellenger NG, Davies LC, Francis JM, et al. Reduction in sample size for studies of remodelling in heart failure by the use of cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2000; 2: 271-8.
- Cesare ED, Giordano AV, Cerone G, et al. Comparative evaluation of TEE, conventional MRI and contrast-enhanced 3D breath-hold MRA in the post-operative follow-up of dissecting aneurysms. Int J Card Imaging. 2000; 16: 135-47.
- Chernoff D, Stark P. Principles of magnetic resonance imaging [online]. UpToDate. [cited 13 July 2006]. Available at URL: http://www.uptodate.com
- Fayad ZA, Nahar T, Fallon JT, et al. In vivo magnetic resonance evaluation of atherosclerotic plaques in the human thoracic aorta: a comparison with transesophageal echocardiography. Circulation. 2000; 101: 2503-9.
- Hornak JP. The basics of MRI, 2006 [online]. The Centre for Imaging Science. [cited 12 July 2006]. Available from URL: http://www.cis.rit.edu/ htbooks/ mri/
- Kanal E, et al. ACR White Paper on Magnetic Resonance Safety: ACR Magnetic Resonance Safe Practice Guidelines. American College of Radiology, 2004.
- Kim RJ, Wu E, Rafael A, et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000; 16: 1445-53.
- Klein C, Nekolla SG, Bengel FM, et al. Assessment of myocardial viability with contrast enhanced magnetic resonance imaging: Comparison with positron emission tomography. Circulation. 2002; 105: 162-7.
- Magnetic Resonance Imaging: Body [online]. Radiology Info. Radiological Society of North America, 2006 [cited 12 July 2006]. Available at URL: http://www.radiologyinfo.org/
- Magnetic Resonance Imaging: Cardiac [online]. Radiology Info. Radiological Society of North America, 2006 [cited 12 July 2006]. Available at URL: http://www.radiologyinfo.org/
- Mahrholdt H, Goedecke C, Wagner A, et al. Cardiovascular magnetic resonance assessment of human myocarditis: A comparison to histology and molecular pathology. Circulation. 2004; 109: 1250-8.
- McCrohon JA, Richmond DR, Pennell DJ, et al. Isolated non-compaction of the myocardium: A rarity or missed diagnosis? Circulation. 2002; 106: e22-3.
- Pennell DJ, Sechtem UP, et al. Clinical indications for cardiovascular magnetic resonance (CMR): Consensus Panel Report. Journal of Cardiovascular Magnetic Resonance. 2004; 6(4): 727-65.
- Plein S, Greenwood JP, Ridgeway JP, et al. Assessment of non-ST segment elevation acute coronary syndromes with cardiac magnetic resonance imaging. J Am Coll Cardiol. 2004; 44(11): 2173-8.
- Reimer P, Parizel PM, Stichnoth FA (editors). Clinical MR Imaging: A Practical Approach (2nd Edition). Heidelberg, Springer-Verlag, 2003.
- Schwitter J, Nanz D, Kneifel S, et al. Assessment of myocardial perfusion in coronary artery disease by magnetic resonance: A comparison with positron emission tomography and coronary angiography. Circulation. 2001; 103: 2230-5.
Dates
Tags
Created by:

 Login
Login