- What is Testicular Cancer (Teratoma of the Testicle)
- Statistics on Testicular Cancer (Teratoma of the Testicle)
- Risk Factors for Testicular Cancer (Teratoma of the Testicle)
- Progression of Testicular Cancer (Teratoma of the Testicle)
- Symptoms of Testicular Cancer (Teratoma of the Testicle)
- Clinical Examination of Testicular Cancer (Teratoma of the Testicle)
- How is Testicular Cancer (Teratoma of the Testicle) Diagnosed?
- Prognosis of Testicular Cancer (Teratoma of the Testicle)
- How is Testicular Cancer (Teratoma of the Testicle) Treated?
- Testicular Cancer (Teratoma of the Testicle) References
What is Testicular Cancer (Teratoma of the Testicle)
A type of testicular cancer is teratoma of the testicle. It is a type of germ cell tumour as it arises from sperm precursors. Germ cell tumours are by far the most common testicular tumours.
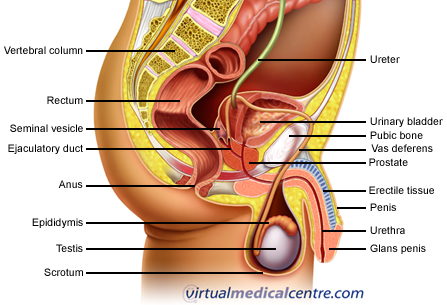
The testes, the paired male gonads, are the sites of spermatogenesis (sperm production). They are ovoid glands consisting of a vast number of coiled seminiferous tubules that join to form the rete testis, which then connect to the epididymis. The testes are located within the scrotum but actually develop on the posterior surface of the abdominal cavity before migrating to their position in the scrotum, through the inguinal canal, during the 7th month of embryological development. Maldescent of the testes (cryptorchidism) is a common condition of neonatal boys, occurring in up to 30% of premature babies and 5% of term infants. The vast majority will descend spontaneously by the age of 1 year. Cryptorchidism is a risk factor for testicular cancer.
Statistics on Testicular Cancer (Teratoma of the Testicle)
Testicular cancer is uncommon, accounting for less than 1% of all malignancies in men but having higher incidences in younger men. Teratoma of the Testicle accounts for 40% of testicular cancers and is most common between the ages of 20 and 30 years but can occur at any age from infancy to adulthood. Geographically, the testicular cancer tumour is found worldwide but with highest incidence in developed countries. Lowest incidence is in African and Asian countries whilst the highest incidence is in Scandinavian countries.
Risk Factors for Testicular Cancer (Teratoma of the Testicle)
- Cryptorchidism: Almost 10% of testicular tumours are found in patients with cryptorchidism (maldescended testes) but this can occur in either of the testes.
- Genetic predisposition- Specific genes have been identified that play a role in testicular cancer.
- Previous testicular cancer
- Family history of testicular cancer
- HIV infection
- Abnormalities of testicular development
- Exposure to oestrogens (female sex hormones) in utero.
- Possible testicular torsion (twisting of the spermatic cord disrupting blood supply to the testes), mumps orchitis, testicular trauma and occupational exposure to chemicals.
Progression of Testicular Cancer (Teratoma of the Testicle)
This type of testicular cancer tumour spreads by haematogenous (blood) and lymphatic routes. Haematogenous spread to the lungs, liver, bone and brain occurs relatively early in the course so many patients may present with already advanced disease. It tends to spread to lymph nodes next to the aorta.
Symptoms of Testicular Cancer (Teratoma of the Testicle)
Your doctor will ask you about your testicular cancer symptoms, past medical history, family and personal history of testicular cancer and previous testicular trauma. The majority of patients present as healthy, in their third or fourth decade of life, with painless enlargement of one testicle.
Clinical Examination of Testicular Cancer (Teratoma of the Testicle)
Your doctor will examine your testicles with you both standing and lying down. The normal testicle is felt first for comparison, then the abnormal testicle will be carefully felt for any lumps or areas of thickening. In addition, lymph nodes in your groin and abdomen will be felt to determine evidence of enlargement from the testicular cancer spreading. Your breast tissue may be examined as gynaecomastia (development of breasts in men) can be associated with several causes of testicular cancer.
How is Testicular Cancer (Teratoma of the Testicle) Diagnosed?
Upon suspicion of testicular cancer or teratoma specifically, your doctor will perform several tests to visualise the tumour and determine the extent of spread. Most testicular cancer patients with a lump or abnormality in the testicles will undergo a scrotal ultrasound which can determine whether the mass is within the testicle and give some details about its consistency. This is followed by radiography and blood tests looking for tumour markers (enzymes and substances released into the blood by tumour cells). Radiographic imaging may include chest x-ray, CT scan of the abdomen, and a CT scan of the chest to determine evidence of metastatic disease.
Prognosis of Testicular Cancer (Teratoma of the Testicle)
As with many malignancies, early diagnosis and intervention are critical to subsequent prognosis in patients with testicular cancer. Improved prognosis occurs with earlier stage at testicular cancer diagnosis, with no non-pulmonary visceral metastases (i.e. spread to other organs besides the lung), and normal levels of serum tumour markers.
Testicular cancer is more aggressive than seminomas, and almost 60% of testicular cancer patients have disease with spread beyond the testis at the time of diagnosis. Testicular cancer overall has become one of the most treatable solid organ malignancies and is associated with a fairly good prognosis. There is a 5 year survival rates for testicular teratoma for approximately 90% in patients with good prognostic features.
In patients diagnosed later in the course of the disease (fewer than 15% of patients) a 5 year survival is only 50%.
How is Testicular Cancer (Teratoma of the Testicle) Treated?
Testicular cancer treatment involves radical surgical inguinal orchidectomy (removal of the testicle) as part of the diagnosis of testicular teratoma- with tissue diagnosis and histological distinction from other forms of testicular cancer being important in subsequent management. Regional lymph nodes may also be sampled or removed during surgery.
Teratoma of the testicle is relatively resistant to radiotherapy but responds well to chemotherapy as an additional testicular cancer treatment to surgery or as a primary treatment in advanced disease. Cisplatin based chemotherapeutic regimes can cure patients with even widespread metastases and other poor prognostic features. You should also be offered the option of semen cryopreservation prior to the commencement of therapy in case you plan to have more children in the future.
Following surgery and/or chemotherapy you will be closely followed to detect any recurrences early. Follow up includes self-testicular examination, measurement of tumour markers in the blood, serial chest x-ray and regular abdominal and thoracic CT scanning. You may also require treatment of specific symptoms from spread of the tumour such as pain from nerve compression and coughing from lung metastases.
Testicular Cancer (Teratoma of the Testicle) References
- Adkins L. Teratomas and Other Germ Cell Tumours. eMedicine. Web MD, 2003. Available [online] from URL: http://www.emedicine.com/ped/topic3023.htm
- Bosl G, Motzer R. Testicular Germ-Cell Cancer. NEJM 1997; 337(4);242-254.
- Burkitt, Quick. Essential Surgery, 3rd Edition, Churchill Livingstone, 2002.
- Cotran RS. Kumar V. Collins T. Robbins Pathologic Basis of Disease. Sixth Edition. Philadelphia: WB Saunders Company; 1999.
- Dearnaley D, Huddart R, Horwich A. Managing testicular cancer. BMJ 2001;322:1583-1588.
- Kumar P, Clark M. Clinical Medicine. Fourth Ed. WB Saunders, 1998.
- Light D. Testicle, Malignant Tumours. eMedicine. Web MD, 2004. Available [online] from URL: http://www.emedicine.com/radio/topic680.htm.
- Hoenig D, Rechtschaffen T. Testicular Tumours: Nonseminomatous. eMedicine. web MD, 2005. Available [online] from URL: http://www.emedicine.com/med/topic3232.htm
- Steele G, Richie J, Oh W, Michaelson D, Clinical manifestations, diagnosis, and staging of testicular cancer, UpToDate, 2006.
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.







