- What is Simple Allergic Conjunctivitis (Seasonal Allergic Conjunctivitis (SAC); Perennial Allergic Conjunctivitis (PAC))?
- Statistics
- Risk Factors
- Progression
- Symptoms
- Clinical Examination
- How is it Diagnosed
- Prognosis
- Treatment
- Simple Allergic Conjunctivitis (Seasonal Allergic Conjunctivitis (SAC); Perennial Allergic Conjunctivitis (PAC)) Prevention
- References
What is Simple Allergic Conjunctivitis (Seasonal Allergic Conjunctivitis (SAC); Perennial Allergic Conjunctivitis (PAC))?
Conjunctivitis is a very common reason for having an uncomfortable, red eye. There are a number of causes for conjunctivitis, including bacteria, viruses and, importantly, allergies.
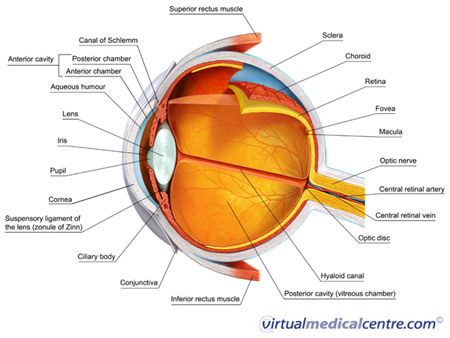
Allergic conjunctivitis affects the conjunctiva of the eye. The conjunctiva refers to the thin, translucent lining of the eyeball and the undersurface of the eyelids.
Simple allergic conjunctivitis appears in two main forms:
- Seasonal allergic conjunctivitis (SAC): A condition caused by allergens which are present seasonally and are most common in spring time. Allergens that cause seasonal allergic conjunctivitis include grass, trees and flower pollens; and
- Perennial allergic conjunctivitis (PAC): A year-round condition caused by allergens found in living environments, including animal fur, dust mites and mould. It is sometimes also caused by allergic reactions to food and/or food additives.
Statistics
Allergic conjunctivitis is extremely common and affects up to 40% of the population. SAC and PAC are by far the most common types of allergic conjunctivitis, and make up the vast majority of all cases. It is estimated that out of all people who experience eye allergies, about 98% will be affected by SAC and PAC.
In children, the condition affects about 17% of 12–13 year olds. Allergic conjunctivitis is often seen in children who have other allergic conditions. For example, 97% of children who have allergic rhinitis (hayfever) also have allergic eye symptoms. In children with asthma, 56% experience allergic eye symptoms, and 33% of children with eczema have allergic eye symptoms. In one large study of asthma and allergies in nearly 500,000 children across several different countries, a slight increase in the rate of allergic conjunctivitis was noted.
In adults, the rates of simple allergic conjunctivitis are highly dependent on the time of year and season.
Risk Factors

The environment also plays a role in the development of allergic conjunctivitis. People are more likely to develop SAC in spring, when there are lots of grass pollens in the air. PAC is associated with common environmental allergens such as dust mites, animal dander and feathers.
Progression
Simple allergic conjunctivitis is often self-limiting, although in some people it may progress to a long-term (chronic) form.
Symptoms
People affected by allergic conjunctivitis usually report a specific set of eye symptoms, including:
- Itching;
- Tearing with a watery discharge;
- Burning;
- Stinging; and
- Mild sensitivity to light (photophobia).
The most common symptom experienced in allergic conjunctivitis is mild itching. Some people may experience intense and intolerable itching, although this is less common. The eyes are generally uncomfortable, but are not normally painful. Your symptoms may get worse in warmer weather, and some people find that nasal symptoms (e.g. itchy or runny nose) accompany their eye symptoms.
It is important that anyone with symptoms of allergic conjunctivitis (e.g. itchy, red or inflamed eyes) visits their doctor to have their symptoms evaluated. The doctor will need to rule out other causes of conjunctivitis, or more serious conditions that may cause uncomfortable red eyes, and will therefore ask detailed questions about the person’s clinical history (that is, their experience of health conditions throughout their life). This will enable the doctor to determine what is causing the allergic symptoms and how the symptoms can best be treated.
If you have eye symptoms or signs, your doctor will pay close attention to several aspects of your history. In particular, they may ask:
- Have you had recent exposure to other people with conjunctivitis or an upper respiratory tract infection? This may suggest a viral cause of conjunctivitis.
- What are the details of your sexual history? In particular, have you had Chlamydia or Gonorrhoea? These can both cause conjunctivitis.
- Are you using any prescription or over-the-counter medications? Some medications can cause inflammation.
- Have you had any eye diseases before, used contact lenses, or had any other conditions that can be associated with eye conditions (e.g. rheumatoid arthritis)?
- Has anyone in your family had allergic conditions (e.g. hayfever, asthma or eczema)?
While all individuals with allergic eye symptoms should consult a doctor, it is particularly important for individuals who have a red eye without itchiness to have their symptoms evaluated by a professional, as the absence of itching indicates the eye condition may have another, more serious cause. It is also very important for those who experience severe, continuous eye pain and/or reduced vision, to seek the advice of a doctor as soon as possible. These symptoms are not typically present in allergic conjunctivitis and may point to a more serious eye condition.
Clinical Examination

The doctor may use an ophthalmoscope to view the back of your eye. The doctor may also use a slit-lamp microscope to see the front structures of your eye. Both of these are painless, routine examinations.
How is it Diagnosed
Often investigations are not required, because allergic conjunctivitis can be diagnosed with the clinical history and examination. However, in some cases the doctor may perform a skin prick test or an allergic challenge test to determine the specific allergen causing the allergic reaction. For example, if the doctor suspects the allergy is cause by animal hair, the individual with allergic symptoms may be exposed to animal hair to see if this makes the allergic reaction worse. If an allergen causing the allergic reaction can be identified, it may be possible for the individual to prevent their allergic symptoms by avoiding the allergen. In this example, if it is found that the allergy is caused by animal hair, then the individual would need to avoid animals and ensure pets are kept out of the house.
Prognosis
In most cases, the symptoms of simple allergic conjunctivitis are mild and long-term treatment is not required. Therefore, the prognosis is favourable. Symptoms can usually be prevented and/or relieved with medication and other measures. However, if left untreated, conjunctivitis can negatively affect quality of life. The condition can be expensive to treat and many individuals pay for at least part of their treatment costs. The condition may also affect daily living.
Children with the condition have poorer school attendance and performance than children who do not. They may also become distressed by the discomfort the condition causes. Adults who experience allergic conjunctivitis work less and have lower incomes than adults who do not experience the condition. They also feel less healthy than do individuals who do not have allergic eye symptoms.
Treatment
Non-pharmacological therapy

Pharmacological therapy
There are a number of different medications that can be used to treat allergic conjunctivitis. The exact treatment plan will depend on the type of conjunctivitis you have and how severe your symptoms are. In many cases, your immediate symptoms will be controlled with a short-term treatment program, followed by a long-term maintenance plan.
If you find your symptoms are not improving or are getting worse despite treatment, you should return to your doctor as soon as possible for a review.
Ocular lubricants
Ocular (eye) lubricants and refrigerating eye drops are usually the first type of treatment the doctor will recommend for individuals with mild to moderate symptoms. Ocular lubricants (e.g. Genteal eye drops or gel (hypromellose) and Cellufresh (carmellose)) are eye drops that lubricate the eye’s surface, making it easier for the eye to remove allergens from its surface.
Decongestants
The symptoms of allergic conjunctivitis arise because the chemicals released in response to the allergic trigger prompt a number of changes and inflammation. The small blood vessels in the eye enlarge, contributing to the redness, itchiness and discomfort experienced.
Decongestants (e.g. Liquifilm Tears (polyvinyl alcohol)) are a type of medication available as an eye drop. They keep the small blood vessels constricted, and so may provide some relief from allergic conjunctivitis. Side effects can occur if these are over-used or are used for a long time, so you should use them according to your doctor’s instructions.
Antihistamines
Many of the symptoms in allergic conjunctivitis are due to histamine. Histamine is released by cells in response to an allergic trigger, and causes itching, enlargement of the blood vessels and a number of other inflammatory changes.
Short-term relief of the itching and redness can be provided by topical antihistamines (eye drops containing antihistamines) (e.g. Livostin (levocabastin)) or oral antihistamines (in tablet form) (e.g. Telfast (fexofenadine), Zyrgic (fexofenadine)). The tablets usually take a couple of days to begin working properly.
Antihistamine agents attach to the same cells in your body as histamine, and in doing so prevent histamine from attaching to these cells. When there is a greater quantity of antihistamine, histamine is unable to bind to cells in the eye. As itching is only triggered when histamine binds to cells, antihistamines prevent or minimise the itchiness, redness and discomfort caused by histamine.
Antihistamine agents are most effective in milder cases of allergic conjunctivitis. They are suitable for short term use (2–6 weeks), but do not prevent future recurrence of symptoms.
Some antihistamines also contain ocular decongestants (e.g. Naphcon A (naphazoline/pheniramine)). These combination medications are more effective than either decongestants or antihistamines used alone. However, they should not be used for more than 14 days.
Mast cell inhibitors
Mast cell inhibiting medications (e.g. Alamast (pemirolast), Alocril (nedocromil), Lomide (lodoxamide)) stabilise cells in the eye known as mast cells, and in doing so prevent the release of histamine and other chemicals that cause the eyes to itch and swell. These medications are used to prevent allergic eye reactions. However, they do not provide immediate symptom relief, usually taking 3–7 days to have an effect.
Mast cell stabilisers/antihistamines
Combined mast cell stabilisers and antihistamines (e.g. ketotifen (Zaditen) and olopatadine (Patanol)) prevent mast cells from opening up and releasing histamine and other chemicals that produce the symptoms of allergic conjunctivitis. They also prevent eosinophils, (cells also involved in inflammation, which contain a red dye called eosin and can stain themselves red) from infiltrating the eyes, thus reducing redness.
These medications provide immediate symptom relief and can prevent the recurrence of allergic eye symptoms. It is usually recommended that mast cell stabilisers be used year-round by people with perennial allergic conjunctivitis. People with seasonal allergic conjunctivitis may stop taking them for a time in winter and autumn, when the allergens that trigger their symptoms are less prominent. These medications effective in most people and generally safe, but like all medications, they should only be used according to your doctor’s advice.
NSAIDS
Topical NSAIDs may be considered in some cases of allergic conjunctivitis, as they reduce itchiness and redness. NSAIDs do this by blocking enzymes involved in producing the chemicals that contribute to allergy and inflammation. Significant side effects can occur with NSAID use, so keep your doctor updated on how your treatment is progressing.
Immunotherapy
Immunotherapy involves giving slowly increasing doses of a specific allergen to a sensitised individual, with the aim to increase their tolerance towards that allergen. Immunotherapy for allergic conjunctivitis has been shown to have a beneficial effect on allergic eye symptoms in some people. However, it is not yet clear how long the effect lasts and whether it is better to give immunotherapy under the tongue (sublingually) or in the skin (subcutaneously.) The effects of immunotherapy on allergic eye symptoms are still being researched and studied.
More information
 |
For more information about allergic conjunctivitis and its subtypes, see Allergic Conjunctivitis. |
Simple Allergic Conjunctivitis (Seasonal Allergic Conjunctivitis (SAC); Perennial Allergic Conjunctivitis (PAC)) Prevention
People who know what causes their allergic conjunctivitis can help prevent the condition by avoiding their triggers. Allergic triggers can be avoided by:
- Using sunglasses to act as a barrier for airborne allergens;
- Using hypoallergenic bedding;
- Washing sheets in hot water; and
- Minimising animal exposure, if animals are believed to trigger allergic symptoms.
People who do not know what causes their allergic conjunctivitis may consider consulting an allergy specialist. The specialist may do allergy testing to identify factors that trigger the symptoms.
There are also medications available which help prevent the symptoms of allergic conjunctivitis. Mast cell stabilising medications (e.g. Lomide (lodoxamide)) are effective in preventing the recurrence of allergic symptoms for up to eight hours after they are taken, but they take 3–7 days to begin having an effect. It is therefore necessary for mast cell stabilising medications to be taken before symptoms occur.
References
- Khaw PT, Shah P, Elkington AR. ABC of Eyes (4th edition). London: BMJ Publishing Group; 2004. [Publisher]
- Leibowitz HM. The red eye. N Engl J Med. 2000;343(5):345-51. [Abstract]
- Bielory L, Friedlaender MH. Allergic conjunctivitis. Immunol Allergy Clin North Am. 2008;28(1):43-58. [Abstract]
- Khurana AK. Comprehensive Ophthalmology (4th edition). New Delhi: Anshan Publishers; 2007. [Publisher]
- Singh K, Bielory L. Ocular allergy: A national epidemiologic study. J Allergy Clin Immunol. 2007; 119(1 Suppl): S154. [Abstract]
- Ono SJ, Abelson MB. Allergic conjunctivitis: Update on pathophysiology and prospects for future treatment. J Allergy Clin Immunol. 2005;115(1):118-22. [Abstract | Full text]
- Hesselmar B, Åberg B, Eriksson B, Åberg N. Allergic rhinoconjunctivitis, eczema, and sensitization in two areas with differing climates. Pediatr Allergy Immunol. 2001;12(4):208-15. [Abstract]
- Gradman J, Wolthers OD. Allergic conjunctivitis in children with asthma, rhinitis and eczema in a secondary outpatient clinic. Pediatr Allergy Immunol. 2006;17(7):524-6. [Abstract]
- Björkstén B, Clayton T, Ellwood P, et al. Worldwide time trends for symptoms of rhinitis and conjunctivitis: Phase III of the International Study of Asthma and Allergies in Childhood. Pediatr Allergy Immunol. 2008;19(2):110-24. [Abstract]
- Bonini S. Atopic keratoconjunctivitis. Allergy. 2004;59 Suppl 78:71-3. [Abstract | Full text]
- Abelson MB, Granet D. Ocular allergy in pediatric practice. Curr Allergy Asthma Rep. 2006;6(4):306-11. [Abstract]
- Moloney G, McCluskey PJ. Classifying and managing allergic conjunctivitis. Medicine Today. 2007; 8(11): 16-21. [Full text]
- Schmid KL, Schmid LM. Ocular allergy: Causes and therapeutic options. Clin Exp Optom. 2000;83(5):257-270. [Abstract]
- Bielory L, Mongia A. Current opinion of immunotherapy for ocular allergy. Curr Opin Allergy Clin Immunol. 2002;2(5):447-52. [Abstract]
- Allergic conjunctivitis [online]. Balgowlah, NSW: Australasian Society of Clinical Immunology and Allergy; January 2010 [cited 2 August 2010]. Available from: URL link
- BMJ Best Practice. Treatment details: Allergic conjunctivitis [online]. London, UK: BMJ Group; 2010 [cited 2 August 2010]. Available from: URL link
- Pitt AD, Smith AF, Lindsell L, et al. Economic and quality-of-life impact of seasonal allergic conjunctivitis in Oxfordshire. Ophthalmic Epidemiol. 2004;11(1):17-33. [Abstract]
- Abelson MB, Ferzola NJ, McWhirter CL, Crampton HJ. Efficacy and safety of single- and multiple-dose ketotifen fumarate 0.025% ophthalmic solution in a pediatric population. Pediatr Allergy Immunol. 2004;15(6):551-7. [Abstract]
- Greiner JV, Mundorf T, Dubiner H, et al. Efficacy and safety of ketotifen fumarate 0.025% in the conjunctival antigen challenge model of ocular allergic conjunctivitis. Am J Ophthalmol. 2003;136(6):1097-105. [Abstract]
- Chapter 11: Eye drugs: Allergic conjunctivitis [online]. Adelaide, SA: Australian Medicines Handbook; July 2010 [cited 10 August 2010]. Available from: URL link
- Product Information: Zaditen. North Ryde, NSW: Novartis Pharmaceuticals Australia Pty Ltd; 27 January 2009.
- Overview of eye allergies [online]. Arlington Heights, IL: American College of Allergy, Asthma and Immunity. March 2009 [cited 17 August 2010]. Available from: URL link
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.







