- What is Liver Cancer (Hepatocellular Carcinoma)
- Statistics on Liver Cancer (Hepatocellular Carcinoma)
- Risk Factors for Liver Cancer (Hepatocellular Carcinoma)
- Progression of Liver Cancer (Hepatocellular Carcinoma)
- Symptoms of Liver Cancer (Hepatocellular Carcinoma)
- Clinical Examination of Liver Cancer (Hepatocellular Carcinoma)
- How is Liver Cancer (Hepatocellular Carcinoma) Diagnosed?
- Prognosis of Liver Cancer (Hepatocellular Carcinoma)
- How is Liver Cancer (Hepatocellular Carcinoma) Treated?
What is Liver Cancer (Hepatocellular Carcinoma)
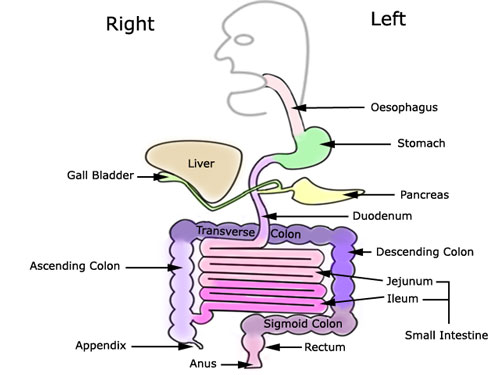
Hepatocellular Carcinoma is a cancer of the liver.The liver is the largest internal organ in the body and is found under the ribs on the right hand side. The functions of the liver are many and varied but can be divided into:
- Protein metabolism – synthesis of circulating proteins and coagulation factors; also involved in protein breakdown;
- Carbohydrate metabolism – regulation of blood sugar level through breakdown and release of stored glycogen or the synthesis of glucose (gluconeogenesis) from protein/fat stores;
- Lipid metabolism;
- Bile formation – bile acids are synthesised from cholesterol in the liver and act as “detergents” to begin the breakdown of fat in the intestine;
- Hormone and drug inactivation – the liver is an important site for the breakdown of hormones produced by the body but is the key organ in the breakdown of alcohol and drugs; and
- Immunological function – the liver plays an important role in protection of the body from bacteria and other antigens from the intestine.
Statistics on Liver Cancer (Hepatocellular Carcinoma)
It is one of the ten most common cancers world wide (although it is relatively rare in the Western world) and occurs with increasing age.
In areas of high incidence it occurs most commonly in the 3rd and 4th decades, but in lower incidence areas it is more likely to occur in the 5th and 6th decades with sex incidence being predominantly male.
Geographically, the tumour is found worldwide, although it is less common in the Western world. There is a much greater incidence in South-East Asia and Africa. The worldwide distribution parallels the distribution of Hepatitis B.
Risk Factors for Liver Cancer (Hepatocellular Carcinoma)
Cirrhosis of the liver (especially macronodular cirrhosis) is the most common predisposing factor worldwide – over 80% of patients with hepatocellular carcinoma will have cirrhosis.
Cirrhosis is commonly due to chronic alcoholism or chronic active hepatitis. a href=”/hepatitis-b-virus/”>Hepatitis B and Hepatitis C virus infection are strongly associated with the development of hepatocellular carcinoma. Rarer cases may be associated with haemochromatosis, aflatoxin (from a fungus), radioactive contrast agent Thorotrast, steroid use and prolonged use of the oral contraceptive pill.
Progression of Liver Cancer (Hepatocellular Carcinoma)
This type of tumour spreads by invasion of blood vessels (either the hepatic or portal vein) with metastases within the liver and, less commonly, to lymph nodes, bone and lung.
How is Liver Cancer (Hepatocellular Carcinoma) Diagnosed?
General investigations may show anaemia and deranged liver enzymes but haematological and biochemical changes are non-specific.
Prognosis of Liver Cancer (Hepatocellular Carcinoma)
Overall the prognosis in most cases of hepatocellular carcinoma is poor with survival rarely more than 6 months from the time of diagnosis. However, with screening of high risk patients there are increasing numbers of smaller, asymptomatic tumours being diagnosed where surgical resection is occasionally possible if the tumour is confined to one lobe. In addition, liver transplantation is an option in cirrhotic patients with a small (<3cm) primary tumour. Overall, cirrhosis is associated with a poorer prognosis whilst encapsulated tumours and the fibrolamellar histological variant may be associated with a better prognosis.
How is Liver Cancer (Hepatocellular Carcinoma) Treated?
Curative treatment can be attempted with surgical resection or liver transplant in patients with early stage disease where tumour size is less than 3cm, and favourable anatomical location determine the likelihood of success.
Radiotherapy may sometimes help pain, especially from the liver capsule.
Systemic chemotherapy for hepatocellular carcinoma has not been very successful. Doxorubicin, cisplatin and 5-FU have been the most succesful drugs, however response rates have been very low (less than 10%) and treatment has had no impact on overall survival. The use of combination chemotherapy has not shown to have any advantage over sigle-agent chemotherapy. Intraarterail chemotherapy (mitomycin, doxorubicin, cisplatin) can be given into the hepatic artery that is providing blood supply to the tumor.
Recently, a new treatment involving administration of radioactive spheres into the liver artery has shown good results. Your oncologist can tell you more.
Improvement in symptoms is an important measurement. Specific monitoring may be by serial measurement of a-fetoprotein or repeat imaging.
The symptoms that may require attention are those of the “paraneoplastic syndrome” often associated with hepatocellular carcinoma. These include lethargy and confusion(hypoglycemia); hypercalcemia, or severe watery diarrhoea.
The tumour may cause visceral pain within the liver itself. If the tumour invades the connective tissue covering of the liver, the liver capsule or ‘Glisson’s Capsule’, it can cause localized somatic pain. See our section on pain in the symptom area.
Sometimes, the pressure within the liver can stimulate the vagus nerve and cause nausea.
Later in the disease, obstruction of the biliary system can cause jaundice and pruritis (itching). Loss of appetite, weight loss and sweating are also common.
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.