ECG/EKG (electrocardiogram)
- What is an electrocardiogram (ECG/EKG)?
- When is an ECG used?
- How to prepare for an ECG
- What can you expect during an ECG?
- What does the ECG record?
- What can you expect after an ECG?
- Interpretation of some possible results
- Ambulatory ECG
What is an electrocardiogram (ECG/EKG)?
The ECG is a graphical recording of the hearts electrical activity during each of its cycles. It is the most common investigation of the heart performed by physicians and is extremely useful.
When is an ECG used?
The ECG is used to investigate suspected problems with the electrical conduction system of the heart as well as some other abnormalities such as metabolic disturbances (e.g. excess potassium). The ECG is an essential tool for health professionals in making a diagnosis of abnormal heart rhythms when one is suspected. It is a routine investigation in people who complain of symptoms such as chest pain as well as breathlessness. The findings of the ECG can also have an effect on treatment of certain conditions, for example it is helpful in deciding some aspects of treatment in people who have suffered from a heart attack.
How to prepare for an ECG
- First reassure yourself that there is no danger or pain involved in performing the procedure and try to relax breathing steadily.
- Rest your arms by your side with your legs flat, making sure that your legs aren’t touching one another.
- Make sure that your chest is exposed as well as your arms and legs.
- The nurse should then clean your skin with a sterile wipe prior to placing the electrodes in place
What can you expect during an ECG?
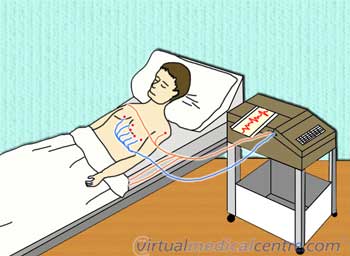
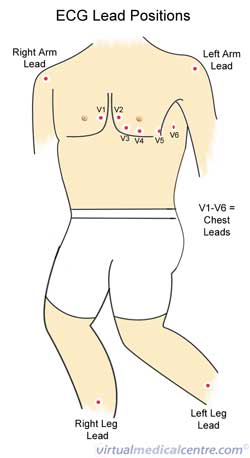
After the preparations that take place before an ECG is performed, various electrodes with a plastic head and an adhesive gel are placed at strategically located points on your body. These points are shown in the diagram to the right, and include:
- 6 points on your chest starting just to the right of your breast bone extending sideways towards the left hand border of your rib cage called V1 – V6.
- 4 points, one on each limb, the ones on the arms are placed below the levels of the shoulders and on the legs they are placed below the level of your groin (note that the closer the electrodes are placed to your heart the more intense the reading is, and the easier it is to interpret).
What does the ECG record?
During the process of the recording the signal is calculated and amplified from the 10 electrodes placed on your body and subsequently recorded on a piece of graph paper with specific dimensions. Depending what ‘lead’ (the vector formed between the different electrodes) you are looking at the ECG appears different. There are 12 such leads in a regular 12 lead ECG, each of which analyse a different plane of the heart and are therefore useful in diagnosing different conditions and localising disease. The ‘leads’ or vectors on the chest wall are named V1, V2, V3, V4, V5 & V6 going from right to left on the patient, and therefore analyse the heart in order from the right to the left i.e. from V1 to V6. The leads on the chest are called unipolar leads because their vector is only pointing in one direction i.e. in a direction perpendicular to the chest wall. There are 4 electrodes on the patients limbs, but only 3 of which are used to form leads and one which is used as an earth, just like the one found on a plug for an electrical device. The 3 limb electrodes used are the right arm, the left arm and the left leg. From these 3 electrodes 6 limb leads are formed, these are named I, II, III, aVR, aVL, and AVF. The leads are formed by using various combinations of the 3 leads, with leads I-III using 2 electrodes to form a vector (bipolar leads) and leads aVR, aVL and aVF using 3 electrodes (augmented bipolar leads).
- Bipolar leads
- I = Right arm to left arm
- II= Right arm to left leg
- III = Left arm to left leg
- Augmented bipolar leads
- aVR = Right arm to left arm and left leg
- aVL = Left arm to left leg and right arm
- aVF = Left leg to left arm and right arm
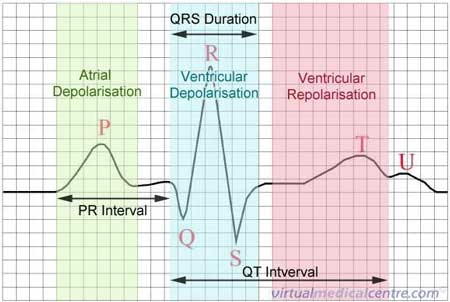
Usually the ECG is recorded on special graph paper that is divided into 1-mm2 boxes. Each box represents a specific time interval since the ECG always records at a particular velocity. By counting these boxes horizontally, the doctor is able to discern the heart rate as well as the timings of the different parts of the ECG. The heart rate, the timings of the intervals (as seen in the diagram below), the height of the recording as well as the leads in which the abnormalities are present all help to make a diagnosis. An ECG readout will look like a series of ‘waveforms’, a single one of which is shown below. The image also highlights the electrical activity in the heart at the time, that causes the distinctive wave. Depolarisation indicates that a wave of electricity has just passed through an area of the heart such as the ventricles of atria, causing them to contract.
What can you expect after an ECG?
After the ECG recording is made, the leads will be removed from your body and the doctor present will attempt to make a diagnosis on the basis of what was found. If the ECG shows a serious abnormality, or there is more information that is needed, other investigations which are more interventional may be indicated, for example an echocardiogram (an ultrasound examination of the heart).
What are some possible results from an ECG and what do these mean?
There are a very large number of possible disorders that can be found on an ECG, but there are some main categories into which a majority of the abnormalities can be grouped.
- Abnormalities of the left heart
- Abnormalities of the right heart
- Abnormalities of the atria
- Abnormally fast rates (tachycardias)
- Abnormally slow rates (bradycardias and conduction blocks)
- Heart attacks
What these abnormalities mean depends on their severity and the patient in question. The diagnosis of an abnormality on ECG does not necessarily mean that an abnormality is present, and if there is an abnormality found that doesn’t correlate with patients symptoms, the ECG should be checked and performed again. It is important to make sure that errors weren’t made in the placement of electrodes or in the interpretation of results, because there is always a margin of error with any investigation.
Ambulatory ECG
Ambulatory ECG monitoring refers to the recording of the hearts electrical activity while a person is active and going about their daily life. This is commonly performed in patients where there is a need to determine associations between what is seen on the ECG and the symptoms that the patient is experiencing.
Indications for ambulatory ECG
An ambulatory ECG is useful for monitoring patients who are at a high risk of heart problems that may not show up in the short space of time that they have in a clinic. It is especially useful for the following peoples:
- Unclear diagnosis: When a clear diagnosis cannot be obtained in the short space of time available in a clinical setting, an ambulatory ECG allows the doctor to gain information about the heart over a whole day, allowing for a much clearer assessment.
- Fainting: Syncope (fainting) and presyncope (lightheadedness) can both be caused by small alterations in heart rhythm that only occur very infrequently. An ambulatory monitor allows these to be picked up due to the length of time it will be monitoring the heart.
- Pacemaker assessment: In people in whom there is a suspected malfunction in a pacemaker, an ambulatory ECG gives detailed information about how the pacemaker is coping with various aspects of day to day life.
- Following a heart attack: After a heart attack, assessing the rhythm throughout the day under various conditions and stresses allows the doctor to have a more accurate picture of how strong the heart is following the infarction.
- Follow-up of abnormal rhythm: Looking at the heart over a longer period of time can help to see if there are any periods of abnormal rhythm that may be missed if an ECG was only conducted in the doctors surgery.
Types of recorders
There are many different types of recorders available, some of which include:
- Continuous full disclosure recording systems: The device can record for 12 or more hours and the whole recording can then be inspected and linked to any signs and symptoms
- Event recorders (memory loop devices): These can be used as an alternative to continuous recorders, especially for patients who experience their symptoms less than once a day. The ECG in these devices is recorded continuously, but is not stored. The patient is asked to activate the device when they are experiencing symptoms in order to store that portion of the rhythm strip. These stored recordings can then be electronically transferred for interpretation.
- Implantable devices: These devices are useful for patients who have infrequent brief periods of arrhythmia which commonly result in syncopal episodes. However these devices should be used generally as a last resort where other investigations have not proved useful.
References
- Guidelines for ambulatory electrocardiographic monitoring [online]. The Cardiac Society of Australia and New Zealand; 2007 [cited 22 January 2007]. Available from: [URL link]
- Hampton JR. The ECG made easy. Nottingham: Churchill Livingstone; 2003.
- Harrisons Chapter 210: Electrocardiography [online]. McGraw Hill. 2006 [cited 22 February 2006]. Available from: [URL link]
- Kumar P, Clark M (eds). Clinical medicine (5th edition). Edinburgh: WB Saunders; 2002.
- Meek S, Morris F. ABC of clinical electrocardiography. Introduction. I-Leads, rate, rhythm, and cardiac axis. BMJ. 2002;324(7334):415-8. [Abstract]
Dates
Tags
Created by:

 Login
Login














