Identifying a suspicious mole (skin self-examination)
- Fast facts about identifying a suspicious mole
- The importance of identifying suspicious moles
- Skin appearance and changes
- Skin self-examinations for skin cancer
- When to see a doctor
- Clinical skin examination for skin cancer
Fast facts about identifying a suspicious mole
- Identifying a suspicious mole early is important because melanoma can spread and become life threatening in as little as six weeks.
- Being familiar with the appearance of your skin is important to help you identify skin changes that may be cancerous.
- Skin self-examination, examining your entire skin surface, is an effective way to identify skin changes that need to be checked by a doctor.
- All Australians should perform regular skin self-examination.
- Skin self-examination should cover the entire skin surface, be performed with the assistance of good lighting, a mirror and if possible another person who can check hard-to-see areas.
- Visit a doctor immediately if you notice moles or spots which are changing or have unusual features including asymmetrical shape, irregular border, blotchy colour, or increasing diameter.
- Take your child to the doctor immediately if they have a new mole or freckle that is pink/red, raised from the skin or bumpy and has a uniform colour.
- If you are at high risk of melanoma, for example because you work in the sun or have previously had skin cancer, have your skin checked by a doctor every six months.
The importance of identifying suspicious moles
 Identifying skin cancer early allows doctors to start treatment quickly and prevent cancer spreading from the skin to the surrounding lymph nodes and/or other organs. Detecting cancerous changes to skin early is the best way to increase the likelihood of successful cancer treatment and survival. Treating skin cancer early also greatly reduces the risk of needing surgery and the potential for disfigurement (e.g. scars on the face from the surgical removal of skin cancers).
Identifying skin cancer early allows doctors to start treatment quickly and prevent cancer spreading from the skin to the surrounding lymph nodes and/or other organs. Detecting cancerous changes to skin early is the best way to increase the likelihood of successful cancer treatment and survival. Treating skin cancer early also greatly reduces the risk of needing surgery and the potential for disfigurement (e.g. scars on the face from the surgical removal of skin cancers).
All types of skin cancers (basal cell carcinoma, squamous cell carcinoma and melanoma) are typically painless. Therefore visual skin checks are the key way of identifying skin changes that may be cancerous. Checking skin regularly is important. While basal and squamous cell carcinoma are rarely life-threatening, melanoma is often life-threatening and can spread very rapidly, in as little as six weeks.
Skin appearance and changes
Being familiar with the appearance of your skin and particularly the nature of irregular features like moles and freckles is an important foundation for identifying cancerous skin changes. Unless you know your skin it will be difficult to identify changes. When checking skin for possible cancer, it is important to check both for new spots and for changes to existing freckles and moles on your skin.
Most people have numerous moles and freckles. They typically develop in the first 15 years of life and appear similar to each other (each person’s moles will be similar in appearance to all their other moles). The average Australian child has about 50 moles by their 15th birthday. While it is normal to have moles, there is an association between higher number of moles and increased risk of melanoma.
Skin self-examinations for skin cancer
Skin self-examination refers to the visual inspection of the entire body for signs of skin changes. It is recommended that all Australians perform regular skin self-examination to ensure cancerous changes to the skin are detected early, before metastasis (spread to other body organs) and when treatment is most likely to be effective. Early detection may reduce the risk of advanced melanoma by more than half because it increases the likelihood that cancerous skin lesions will be identified when they are still relatively small (≤1mm thick). Approximately half of all melanomas are diagnosed after people visit their doctor to check suspicious skin changes they identified while doing a skin self-examination.
Regular skin self-checks play a crucial role in detecting skin cancer early and preventing disfiguration caused by surgery and death. Skin cancer lesions are usually visible to the naked eye and regular self-examination for skin changes can often identify changes which may be indicative of cancer and need to be checked by a doctor.
Who should perform skin self-examination?
Regular skin self- examination is recommended for all Australians, but particularly for individuals:
- Aged 40 years and above;
- Working outdoors;
- With a personal or family history of skin cancer.
In practice just over half of Australian adults (56% of men and 61% of women) check their skin regularly.
Skin self-examination may be easier with the help of your partner, a close friend or carer. Talk to your doctor about information that may assist you and your helper to identify any skin changes. Your doctor may also be able to advise you about how to document skin changes so you can keep track of them over time.
How often should skin self-examination be performed?
All Australians should perform regular skin self-examination to identify skin changes.
People who have a high risk of melanoma should perform skin self-examination every three months. These include people who spend a lot of time in the sun, those who have had skin cancer, those with family members who have had skin cancer and those with fair skin and numerous freckles and moles.
How to perform a skin self-examination
Where to examine
All the skin is potentially at risk of skin cancer, even sections of skin which are rarely exposed to the sun. These include the soles of the feet and palms of the hand, as well as areas of skin usually covered by clothing. Check your entire skin, including areas not commonly exposed to the sun such as the soles of the feet, palms of the hands and areas normally covered by clothing. Also be careful to check areas of your body that are not easy to see like the back of your neck.
Using mirrors
If possible get someone (e.g. your partner) to help you check areas of your skin which are difficult to see, even with a mirror.
If you are checking your skin alone a full length mirror is essential for skin monitoring. A hand held mirror will also be needed so you can see areas of your skin which remain hidden in the mirror.
To perform a skin self-examination stand naked in front of the mirror. Good light is essential. Using the mirror check all areas of the skin. The hand mirror should be used to help you see areas like the back of the neck.
Recording information
Record the date on which you perform each examination and note the skin areas and lesions you are monitoring. Photographing skin lesions or areas of skin may be a useful way to keep track of skin changes overtime. Don’t forget to date the photographs you take.
When to see a doctor
Red flags in adults
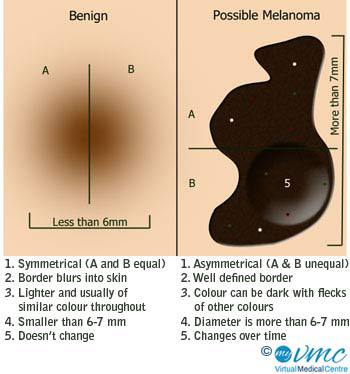
New skin lesions and changes to existing skin lesions (e.g. increasing size or change in colour) may indicate cancerous changes and should be checked by a health professional. Assessing skin lesions for ABCD characteristics may help you identify skin lesions features associated with skin cancer.
These are:
- Asymmetry or a skin lesion which does not have the same shape on both sides when a line is drawn through the middle.
- Border Irregularity that is a mole with a border that looks different in different places.
- Colour which varies, that is there are several different colours within a single lesion or the mole is changing colour (e.g. from brown to black).
- Diameter or size increasing.
You should visit your general practitioner for a skin check if you notice:
- New lesions (moles or freckles).
- Old skin lesions which have increased in size since your last skin examination.
- Notches or small bumps appearing on the border of a mole.
- A spot or mole changing colour, for example from black to brown.
- A spot or mole which raises from the skin or has a raised lump within it.
- Moles which develop a rough, scaly or ulcerated surface, or begin bleeding or weeping.
- Unusual sensations on the skin of moles or spots for example itching or tingling.
- Spots that are visibly different from other moles or spots on your body which may be thought of as ‘ugly ducklings’.
Seeking immediate assessment with a general practitioner or at a specialised skin cancer clinic is vital if you notice any of these skin changes. Early treatment, before regional spread or metastasis significantly improves five-year survival following melanoma treatment to 96% (compared to 34% with metastasis and 63% with regional spread).
Red flags in children
In children melanoma lesions usually have different characteristics to the typical ABCD characteristics of adult lesions. Modified ABCD criteria have been developed to assist in the diagnosis of melanoma in children. These are:
- Amelanotic: typically melanoma lesions in children are amelanotic meaning that they do not contain the pigment melanin and are thus a red or pink colour (rather than black or brown like adult spots).
- Bleeding and bumpy: melanoma in children usually appears as raised bumps on the skin. They often bleed.
- Colour: in children melanoma lesions usually have a uniform colour.
- Diameter: melanoma lesions in children are usually less than 6mm in diameter. They are usually new lesions, not existing moles or spots which have changed colour or shape.
Clinical skin examination for skin cancer
In addition to seeing a doctor when suspicious skin changes are identified through self-examination, individuals with a high risk of melanoma should have their skin visually checked by a health professional every six months. The doctor may use full body photography and/or dermoscopy (a special device used to visualise skin close-up) to help them examine and document the skin lesions.
Assessment by a health professional is necessary to diagnose or rule out skin cancer when suspicious skin changes (red flags) are noticed during skin self-examinations. However regular skin examination by a health professional is not recommended for all Australians. Unless you are at high risk of skin cancer, you only need your doctor to check your skin if you notice suspicious changes.
More information
 | For more information on this type of skin cancer, including its staging, prevention, possible treatments, and other useful resources, visit Melanoma. |
References
- Cancer Council Australia. Check for Signs of Skin Cancer. 2014. (Cited 13 October 2014). Available from: [URL Link]
- Sun Smart Victoria. Skin Cancer Types. 2014. [cited 3 December 2014]. Available from: [URL Link]
- National Health and Medical Research Council. Clinical Practice Guidelines for the Management of Melanoma in Australia and New Zealand. 2008. [cited 13 October 2014]. Available from: [URL Link]
- Cancer Council Australia. Skin Cancer Issues and Statistics. 2014. (Cited 13 October 2014). Available from: [URL Link]
- Cancer Council NSW. Skin Cancer Screening. 2013. (cited 13 October 2014). Available from: [URL Link]
- Cancer Council Australia. Skin Cancer Statistics and Issues- Detection and Screening. 2014. [cited 3 December 2014]. Available from: [URL Link]
Dates
Tags
Created by:

 Login
Login