- What is Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
- Statistics on Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
- Risk Factors for Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
- Progression of Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
- Symptoms of Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
- Clinical Examination of Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
- How is Medulloblastoma / Primitive Neuroectodermal tumour (PNET) Diagnosed?
- Prognosis of Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
- How is Medulloblastoma / Primitive Neuroectodermal tumour (PNET) Treated?
- Medulloblastoma / Primitive Neuroectodermal tumour (PNET) References
What is Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
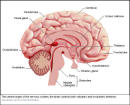
The brain is contained within the cranial vault, and is divided into several sections by folds of dura mater (one of the three membranes encasing the brain). The posterior fossa of the skull contains the cerebellum and brainstem.
The term primitive neuroectodermal tumour or PNET is a relatively new term that is used to describe a group of tumours. In these tumours, the type of cell seen is very similar. Their locations are quite different. Tumours that fall under the heading PNET include medulloblastoma (the most common), pineoblastoma, ependymoblastoma, retinoblastoma, neuroblastoma and esthesioneuroblastoma. Other than the medulloblastoma, these are all rare tumors. These tumors generally occur in children.
Statistics on Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
Medulloblastomas the most frequent malignant brain tumour occurring in children.They account for 20% of all childhood brain tumours and 50% of cerebellar tumours in children. In contrast, only 1% of brain tumors in adults are medulloblastomas.
50% occur in the fist decade of life, however, a second smaller peak occurs in adults between the 2nd to 4th decades of life. These tumors are slightly more common in males than in females.
Risk Factors for Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
As for most brain tumours the cause of medulloblastoma is unknown. However, like all other brain tumours, there are a few known risk factors:
Progression of Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
Medulloblastomas initially grow into the cerebellum – the past of the brain that controls balance and posture. After this they may spread via the cerebrospinal fluid (CSF) into the spinal cord.
As the tumour grows it may block the flow of CSF, leading to the development of hydrocephalus (increased head size caused by increased fluid in the brain) in young infants and children, or raised intracranial pressure in older children and adults.
Other complications include post-operative infection, paralysis, nerve palsies, cognitive dysfunction and growth retardation.
How is Medulloblastoma / Primitive Neuroectodermal tumour (PNET) Diagnosed?
- There are usually little to note on laboratory examination in brain tumours.
- A lumbar puncture may reveal malignant cells and a raised pressure in the brain.
Prognosis of Medulloblastoma / Primitive Neuroectodermal tumour (PNET)
Provided the tumour is not widespread at diagnosis, it is often responsive to treatment, otherwise it is quite an aggressive tumour with a poor outcome. More than 70% of children survive longer than 5 years after diagnosis.
How is Medulloblastoma / Primitive Neuroectodermal tumour (PNET) Treated?
The treatment for medulloblastoma depends on a number of factors including the general health of the patient and the size and position of the tumour.
Medulloblastomas occur much more commonly in children than adults, and treatment is not without risk. There may be some long-term effects of treatment including growth and hormonal changes, behavioural changes and possible learning problems, and these need to be discussed with the treating doctor.
Where possible, the bulk of tumour is removed by surgery. Further brain scans may be performed to assess how much of the cancer is remaining, and this is treated either with radiotherapy, chemotherapy, or both.
Medulloblastoma / Primitive Neuroectodermal tumour (PNET) References
- Braunwald, Fauci, Kasper, Hauser, Longo, Jameson. Harrison’s Principles of Internal Medicine. 15th Edition. McGraw-Hill. 2001
- Cotran RS, Kumar V, Collins T. Robbins Pathological Basis of Disease Sixth Ed. WB Saunders Company 1999.
- Hankey G., Wardlaw J. Clinical Neurology. Demos Medical Publishing, United Kingdom, 2002.
- Kumar P, Clark M. Clinical Medicine. Fourth Ed. WB Saunders, 1998.
- Oxford Textbook of Oncology (2nd edition). Souhami et al. Oxford University Press, 2002.
All content and media on the HealthEngine Blog is created and published online for informational purposes only. It is not intended to be a substitute for professional medical advice and should not be relied on as health or personal advice. Always seek the guidance of your doctor or other qualified health professional with any questions you may have regarding your health or a medical condition. Never disregard the advice of a medical professional, or delay in seeking it because of something you have read on this Website. If you think you may have a medical emergency, call your doctor, go to the nearest hospital emergency department, or call the emergency services immediately.







